Epiretinal Membrane
Eye Conditions
Cataract
CSCR
Diabetic Retinopathy
Epiretinal Membrane
Flashes and Floaters
Glaucoma
Macular Degeneration
Macular Hole
Retinal Detachment
Retinal Vein Occlusion
Uveitis
Vitreomacular Traction
Investigations
Procedures
Epiretinal membrane is the build-up of scar tissue on the surface of the macula. As the membrane thickens, the macula becomes swollen and wrinkled, leading to blurring of vision and distortion of images.

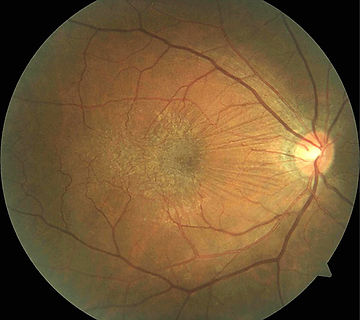
White scar tissue
Stretch lines
on macula
OCT Scan

Cross section view of normal macula

Leads to
Blurring and distortion of images
Cross section showing thickened and distorted macula
Epiretinal membrane is treated by vitrectomy surgery. The surgery is performed under local anaesthesia with minimal discomfort. With modern techniques, sutures are usually not required.

Vitreous is removed through tiny cuts on the sclera (white of eye) using an automatic cutter.
Epiretinal membrane is stained with a dye and peeled off from the macula using fine forceps.
What is epiretinal membrane?
Epiretinal membrane, also commonly called 'macular pucker', is the build-up of a thin layer of scar tissue on the surface of the macula. Like all scars, epiretinal membrane contracts and causes the underlying macula to become swollen and wrinkled. People with epiretinal membrane notice blurring and distortion of their central vision. Since the peripheral vision is not affected, it does not lead to total blindness. However, severe epiretinal membrane can reduce the vision to the level of legal blindness (less than 6/60).
Who are affected?
Epiretinal membrane is mostly seen in people over the age of 50, but it can occur in younger individuals. It affects around 5 to 10 % of Australians over 50 years of age. Men and women are affected equally.
What causes epiretinal membrane?
The cavity inside the eye is filled with a gel-like substance called the vitreous. In youth, the vitreous is stuck to the surface of the retina. With aging, the vitreous shrinks and separates away from the retina. Irritation of the retina during the vitreous separation can cause inflammation that leads to scar formation on the macular surface. Bits of vitreous can remain stuck on the surface of the macula and organise into scar tissue.
Certain eye conditions, such as diabetic eye disease and uveitis, can lead to epiretinal membrane formation. Major trauma to the retina, e.g., retinal tear or detachment, are also known causes of epiretinal membrane.
How is epiretinal membrane diagnosed?
Although epiretinal membrane can be seen through the examination microscope, OCT scan has become the standard for its diagnosis and evaluation. OCT scan uses computer-controlled laser beams to build cross-sectional images of the macula, offering highly detailed view of its structure. Fluorescein angiography may be performed to assess the retinal circulation and to exclude other causes of macular swelling or wrinkling.
When should epiretinal membrane be treated?
Most epiretinal membranes do not require treatment. Surgery is recommended when the membrane causes significant blurring or distortion of vision, or if the membrane has been shown to worsen with time. Ongoing follow-up is needed to determine whether the epiretinal membrane is getting worse. Visual results are best when the surgery is performed early, before the macula becomes severely distorted and the vision has deteriorated.
How is epiretinal membrane treated?
Epiretinal membrane is treated by a technique called vitrectomy. Modern vitrectomy technique uses tiny wounds and usually do not require sutures. Three small wounds are made on the white part of the eye, through which an infusion tube, light source and vitrectomy cutter are inserted. After the removal of the vitreous gel, the membrane is identified by staining it with a dye. The membrane is then removed using a pair of fine forceps. If the retina becomes unstable, a bubble of air or gas may be injected into the eye cavity.
What are the benefits and risks of having surgery for epiretinal membrane?
The aim of the surgery is to stabilise the vision and prevent further damage to the macula. Most patients perceive an improvement in distortion symptoms, and the visual acuity improves in 2 out of 3 patients. It takes around 4 weeks for the vision to start recovering, and the improvement can continue beyond one year after the surgery. Because some wrinkling and swelling of the macula persist after the surgery, it is usually not possible to achieve a completely normal vision.
Overall risk of complication is low, but can include the following:
-
More common: Cataract, persistent macular swelling
-
Less common: Retinal detachment, high eye pressure, temporary bleeding, recurrent membrane
-
Rare: Infection, severe bleeding, unexplained poor vision
Cataract can develop months or years after the vitrectomy and will require surgery. Cataract refers to the lens inside the eye becoming hazy. Modern surgical techniques have made cataract surgery safe and efficient. The delicate retina can be injured during vitrectomy and result in a retinal tear or detachment. Retinal tears found during the surgery will be treated immediately, but if the retina becomes detached after the surgery, a second procedure will be needed to repair it. As for all eye surgeries, bleeding and infection are rare possibilities. It is unusual for epiretinal membrane to recur.