Cataract Surgery
Eye Conditions
Cataract
CSCR
Diabetic Retinopathy
Epiretinal Membrane
Flashes and Floaters
Glaucoma
Macular Degeneration
Macular Hole
Retinal Detachment
Retinal Vein Occlusion
Uveitis
Vitreomacular Traction
Investigations
Procedures
Cataract refers to fogging or clouding of the crystalline lens. Vision gradually becomes more blurry, and images lose clarity and colour. You may feel more glare on bright sunny days and lights may appear streaked at night.
In this section, we will discuss the details of cataract surgery. To find out more about cataract as an eye condition, please read the section on Cataract.
Cataract surgery has had a long evolution, beginning in the ancient times with a technique called "couching" where a needle is used to dislodge the clouded lens into the vitreous. Remarkably, couching is still practiced in some parts of the world today. Surgical techniques thankfully have improved enormously, especially over the past 50 years with the introduction of phacoemulsification (phaco). This technique uses an ultrasound device to break up the clouded lens, which are vacuumed out through a tiny wound. Prior to phaco, cataract was removed manually through a large wound. Excellent visual results were achieved but larger wounds meant slower recovery and more discomfort.
Modern cataract surgery not only benefits from sophisticated phaco systems, but also the advances in artificial lens technology, and instruments to measure the size and curvature of the eye prior to surgery to predict the visual outcome more precisely. This means that cataract surgery is no longer performed only to reverse vision loss, but also offers the opportunity to correct any focus error the patient has (i.e., short sightedness, long sightedness, astigmatism). More recently, laser has been introduced to allow a more accurate construction of wounds but it has not yet been shown to improve visual outcome.
Intraocular lens
Phaco handpiece
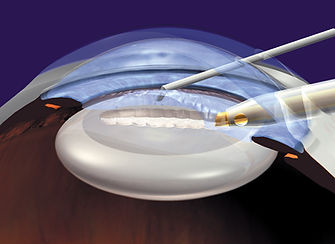
Phaco surgery is performed under a local anaesthesia, which can be given as an injection around the eye or as eye drops for suitable patients. A small wound is made at the edge of the cornea measuring around 2.5 mm for the phaco instrument. The wound is constructed obliquely so that it will seal without stiches. One or two other tiny wounds are made for accessory instruments. The anterior chamber is filled with surgical gel for stability and a round opening is made in the front part of the lens capsule, which is the skin that covers the natural lens. The aim is to remove the internal lens matter but preserve the capsule, which will act as the holder for the new artificial lens.
Using the phaco instrument, the internal lens matter is broken up into small pieces and vacuumed out. Lens residue on the capsule is removed using a vacuum probe. The lens capsule is now an empty bag, into which the artificial lens is inserted, taking care that it is well centred. Remaining surgical gel is removed from the anterior chamber and the corneal wounds are checked for leakage.
Phaco surgery
Warning: Clinical surgical footage
Recovery from phaco surgery is usually rapid. The vision is likely to be slightly blurred the next day but should be adequate for normal activities. Some gritty irritation is to be expected but severe pain is highly unusual. Surgery inevitably causes inflammation and swelling, and the cut in the cornea subtly alters the shape of the eye. As the swelling settles and wounds heal, vision will become sharper. Floaters may become more noticeable. These are mostly harmless but if the floaters suddenly worsen, especially if there are also flashes in the periphery of vision, an urgent inspection of the retina is needed.
Most people do not wear glasses for long distance vision and choose to remain so after cataract surgery. For people who are naturally short (myopic) or long (hyperopic) sighted, the power of the artificial lens can be adjusted so that they can achieve good long distance vision without glasses. Many short-sighted people wish to retain their ability to read without glasses. Again, the appropriate choice of artificial lens power will allow them to achieve this. For people with astigmatism, special lenses with astigmatic correction can be used.
Most artificial lenses are single focus, meaning that if the patient has good distance vision, glasses will be needed for reading. Multifocal artificial lenses have been introduced to provide a broader range of focus but there are significant compromises that need to considered carefully. This includes unwanted perceptions such as haze, haloes and streaks, as well as gaps in focus at different distances. Furthermore, the shape of our eyes undergo changes just like other parts of our body, and what was initially in clear focus may become blurred over time.
Cataract surgery is undoubtedly safe and refined but no surgery is without risks. If the delicate lens capsule becomes torn during the surgery, the artificial lens will need to be inserted between the iris and capsule, or in front of the iris. The zonules, which are fine fibres that hold the lens suspended, may be weakened so that the capsule is not stable enough to hold the lens implant. The artificial lens can become dislodged from its desired position and affect the visual outcome. A mild leakage from the wound seals spontaneously, but if internal tissues become trapped in the wound, they need to be released surgically. Macular swelling can develop in a small proportion of patients and may require additional treatment if it persists. The lens capsule can become cloudy months or years after the surgery and cause symptoms identical to cataract. This is readily dealt with using a short laser procedure in the clinic (See Yag Laser).
If lens fragments get dislodged into the vitreous during the surgery, they will need to be removed through an additional surgery. Retinal detachment, like-wise, requires a second surgery to repair it. Infections can occur despite all precautions, but it is thankfully rare, with risk of 1 in 2000. Severe bleeding is also rare.